
Photoacoustic Mammoscopy for evaluating screening-detected lesions in the breast
Background
Effect
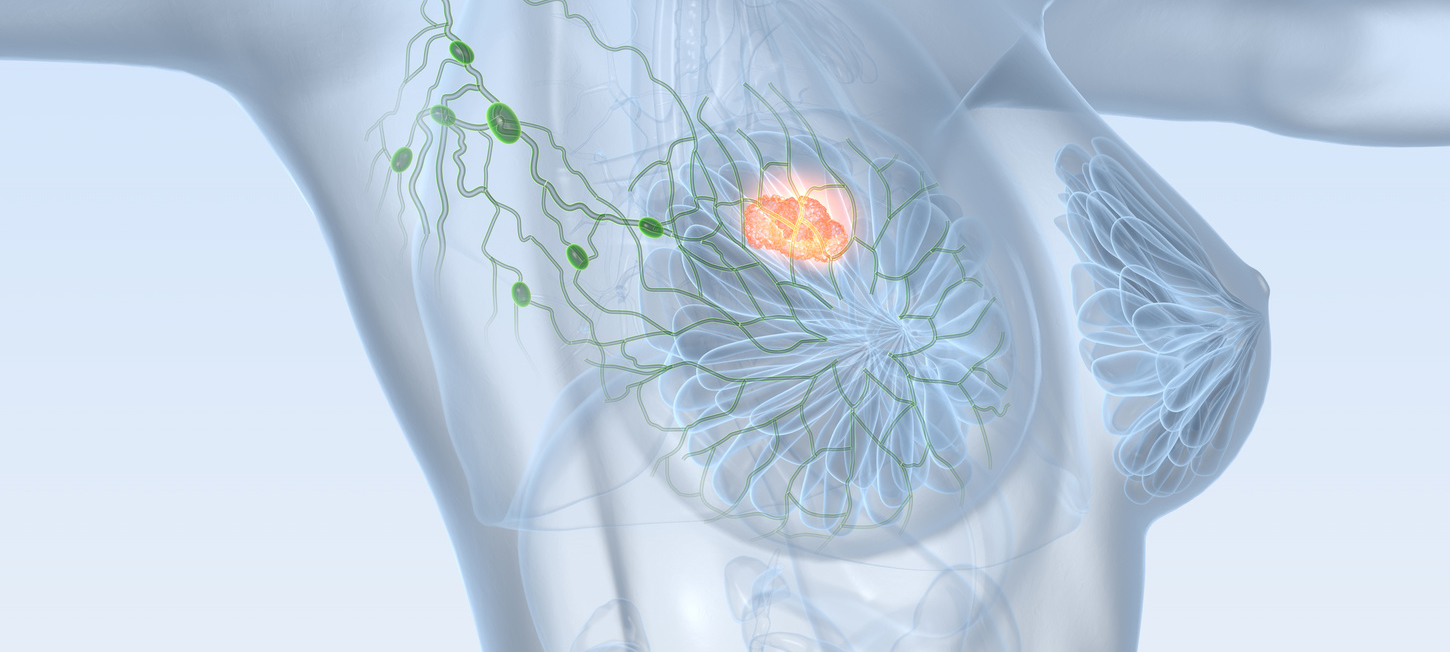
In 2012, 1.7 million women were diagnosed with breast cancer worldwide, and about 0.52 million women died from the disease. [Torre et al 2015] Breast cancer alone accounts for 25% of all cancer cases and 15% of all cancer deaths among females.[Torre et al 2015] Early detection and accurate diagnosis are crucial for optimizing survival chances with appropriate therapy. X-ray mammography, the only technique found sensitive enough for screening has a low positive predictive value (PPV) with unnecessary secondary investigations including biopsies. It has been estimated that 20-50% of abnormal mammograms in screening will prove to be negative. [Stout et al 2014] Most patients referred to a specialized breast cancer care center after a positive screening will have benign disease. [Kopans 2006]
Diagnosis
The paradigm in diagnosis is to establish whether a screening-detected lesion is a cancerous mass or a benign process, leading to vastly different therapeutic decisions. Diagnosis is performed using x-ray imaging, ultrasonography and image-guided needle biopsy. [Kopans 2006] Depending on availability, Magnetic Resonance Imaging (MRI) may be used in case of uncertain findings in x-ray imaging and ultrasound imaging. [Kuhl 2007]
Weak points
Despite advancements, these clinical imaging modalities still have much room for improvement.
In addition to specific drawbacks for each method, the interaction of the interrogating energy – whether x-rays, ultrasound or radiofrequency waves (in a magnetic field) – with the malignancy is often not sufficiently specific to allow discrimination of the malignancy from healthy tissue or a benign abnormality. This results in recourse to multiple and/or repeat imaging, and often unnecessary biopsy. The consequences of the shortcomings are often physical, psychological and economic burdens felt at individual, familial and societal levels.